Mediastinal emphysema caused by a dental laser
Keywords:medical fibers, laser applications, Time:10-08-2016Antibiotics were administered prophylactically for several days. After 6 days from the onset, the patient’s emphysema had resolved without any complications.
1. Introduction Iatrogenic emphysema caused by dental treatments is uncom- mon. Dental treatment using an air turbine drill and a three-way syringe for exodontia and in the treatment of caries, and the use of hydrogen peroxide for root canal treatment have been reported as major causal factors . We report a case of mediastinal emphy- sema caused by dental laser use and discuss the possible pathology of emphysema.
2. Case report A 64-year-old female presented to the emergency unit in our hospital with the complaint of swelling of the right cervix and face in October 2006. Initially, she noticed a gum abscess on the right upper first premolar gum and went to see a dentist. After the dental examination her dentist diagnosed her condition as a gum abscess due to a root fracture on the right upper first premolar tooth and considered drainage. He made an incision using a den- tal laser on her buccal mucosa under local anaesthesia. During the treatment, she felt a sense of being oppressed in the region and extended to the neck and chest. She told her dentist that she was experiencing a sensation of suffocation. Swelling on her right face was observed when the dentist stopped the treatment. The den-tistsuspectedsubcutaneousemphysemaandmassagedtheregions of swelling, but this was not effective. He then stopped massag- ing and gave instructions for rest and prescribed an antimicrobial. After returning home, the patient had chest pressure and vomited three times. She became anxious and went to see another doc- tor in a local private hospital. When a physician examined her, he decided to refer her to an oral surgery unit for special con- sultation, and she came to our hospital on the night of the same day.
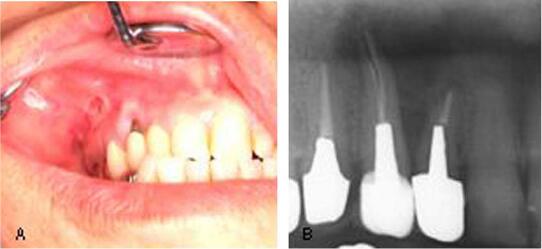
A physical examination revealed trismus and dysphagia with diffuse swelling from the right temporal region to the precordium ( Fig.1 ).Sinceminorchestpainhadoccurred,weperformedanelec- trocardiogram test, however, there were no abnormal findings. At the time of this examination, she was unable to open her right eye, and crepitations were found upon palpitation of the swelling. In the oral examination, we observed surgical wounds in the apical area on the upper first premolar tooth on the right side ( Fig. 2 A). The dental X-ray showed the root fracture and corresponding radiolu- cent area of the tooth ( Fig. 2 B). Based on the patient’s explanation, the wounds seemed to be from a laser radiation trace. There were no abnormal findings such as redness, swelling and pain in the wound. A chest X-ray showed evidence of subcutaneous and medi- astinalemphysemaontherightcollarbone( Fig.3 ).Usingcomputed tomography, transmitted images that seemed to be an atmospheric layer, were found in the right buccal space, masticator space, parotid space, parapharyngeal space and retropharyngeal space on the contralateral side ( Fig. 4 ). These shadows extended to the upper mediastinum ( Fig. 5 ). Blood and biochemical examinations showed that C-reactive protein (CRP) levels were increased to 1.0mg/dl, but other tests were within normal limits. From these findings,we diagnosed her condition as mediastinal and subcutaneous emphysema.
On the same day that the patient was hospitalised, we admin- istered prophylactic antimicrobial agents (FMOX 2g and CLDM 1200mg/day). On the third day, subcutaneous emphysema in the patient’s right masticator space, as well as pain in swallowing, were decreased. However, her submandibular and thoracic crepi- tations seemed to have extended downward. On the 6th day, she was able to open her mouth wider with reduction of her facial swelling although her upper chest and temporal crepitations were still slightly apparent ( Fig. 6 ). Since CT scan images showed that the emphysema had improved with normalised values of CRP and other laboratory tests, we discharged the patient.
3. Discussion Subcutaneousemphysemaisaconditioninwhichairpenetrates the subcutaneous tissues, and mediastinal emphysema is where air accumulates in the mediastinum, which is located in the middle of the chest and divides the right and left chest. Since mediastinal emphysema may cause dyspnea and acute mediastinitis, careful observation with X-ray images and prompt diagnosis are required [5] . It has been reported that approximately 50% of emphysema is overlooked by chest fluororoentgenography [6] , and a CT scan examination is required if emphysema is suspected. With regard to the clinical manifestations of mediastinal emphysema, primary chestpainshouldbedifferentiatedfromischemicheartdiseaseand other mediastinal diseases. There are various causal factors for cervical subcutaneous emphysemasuchastrauma,exercise,bronchialasthmaandcough- ing. Mucosal injuries in areas such as the pharynx, larynx and oesophagus are the common causes of mediastinal emphysema [5] . There is also a known possibility that dental treatment can cause emphysema [7] . It is believed that mediastinal emphysema may occur regardless of the size of subcutaneous emphysema when facial or cervical subcutaneous emphysema is caused by dental treatment. It has been reported that the most common localisation for emphysema in the oral cavity is the third molar in the lower jaw followed by the upper cuspid, premolar and lower molar parts [8] . Recently leaser treatment is becoming more common in dentistry periodontal treatment, caries treatment, root canal treatment, den- talimplantandothersoralsurgeries [9,10] .Therehavebeenseveral casereportsshowingthatemphysemaoccurswithCO 2 laserusefor cutting in neck surgeries [4,11,12] . However there has been little reported on the development of mediastinal emphysema by dental treatment [3] , and this is the first report of mediastinal emphysema caused by use of a YAG laser during dental treatment in general dental practice.
Dental laser produces compressed air same as a turbine and a three-way syringe. We speculate that in this case, compressed air was the main causal factor for subcutaneous and mediastinal emphysema. According to a dental laser manual, the method of incision is to first cut the part of the swollen gum for opening with a laser and to secure drainage. In addition, the laser should be used without fixing the tip in the same location while putting a tip in and out when the laser is used in submucous tissues. In most den- tal chairs, the air pressure of the air turbine is set at 5.0–5.9kg/cm 2 .On the other hand, according to the user’s manual, the air pressure of the dental laser in this case was 3.0–4.0kg/cm 2 , which is lower than that of the air turbine. The length of time that the tip was inserted might also be related to the emphysema outbreak. With regard to the penetration course of the subcutaneous and mediastinal emphysema anatomically, the distance from the api- cal area to the buccal bony wall is approximately 2–3mm, and air is likely to penetrate the submucosal space. We assume that the air could have been spread first from the mucosal bottom of the first premolar tooth to the masticator space followed by the submandibular space, temporal space, anterior neck space and mediastinum. In the case of maxillofacial infections, inflammation is spread deep into the parapharyngeal space from the mastica- tor space to the mediastinum through the cervical part containing potential spaces between layers of muscles, organs and other struc- tures [13] . In our case, we speculate that the emphysema of the retro-pharyngeal space spread to downward direction and leading to the mediastinum even passing thorough the contralateral para- pharyngeal space. Furthermore, physical stimulation by massaging the swollen part of the face after the onset of the emphysema might have spread the air to other anatomical spaces. Conservative treatment is recommended for mediastinal emphysema so that the air will absorb spontaneously. It is likely that mediastinitis may be caused by bacteria in the oral cavity throughemphysema [14] .Whenmicroinfectionoccursinthemedi- astinum and subsequent mediastinitis emerges, it is important to consider the prompt initiation of mediastinum drainage. To pre- vent an outbreak of subcutaneous emphysema, further education of how emphysema can be caused and correspondence for compli- cations is necessary for those dentists who commonly use laser devices in private practice. Further development of a laser that exerts weak pressure is also required to reduce the risks of surgical complications by the medical equipments.
4. Conclusion Weexperiencedacaseofmediastinalemphysemathatoccurred during dental laser treatment. It is necessary to be aware of the possibility of subcutaneous and mediastinal emphysema onset at the time of laser treatment. This condition needs to be carefully managed, particularly in the areas most vulnerable to emphysema.We thank the patient for participating in this study as well as the following clinicians for referring the patient.
Related Articles
- Laser Therapy in the Treatment of Dentine Hypersensitivity
- Low level laser therapy in dentistry
- Disposable bare fiber in oral and facial practice
- Pulsed Nd:YAG Laser Treatment for Failing Dental Implants Due to Peri-implantitis
- Laser Fibers Application in Periodontics
- Laser Treatment for Failing Dental Implants
- Medical fibers:A New Approach to Relieve Pain in Some Painful Oral Diseases
- The TwinLight™ Concept in Dentistry Reviews
- Er:YAG laser applications in dentistry
- Dentine Hypersensitivity medical Laser fibers Therapy
